This was written by Hans Helseth, with Ken Grauer, and a bit of help from Smith
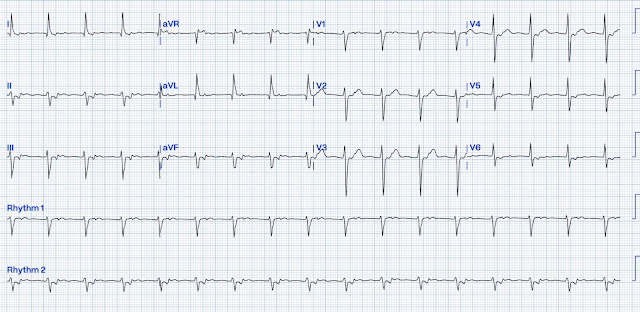
Without any patient information, how might you interpret this rhythm?
This is a supraventricular rhythm. There is a regular narrow complex tachycardia at a rate of 118 BPM with a normal axis.
Below is a lengthy discussion of the diagnosis of this rhythm. But we in Emergency Medicine don't always need to know the diagnosis, just what to do. For that see the very end of the discussion.
Atrial activity may not be immediately apparent, but close attention the inferior leads reveals negative P waves hidden within the ST segments. In V1, small high frequency upright P waves are also visible. We can surmise that these are P waves, and not part of the ST-T complex, because of their high frequency. T waves usually have smoother ascents and descents, while P waves have a shorter duration and appear "sharper" on the EKG.
The negativity of the P waves in inferior leads suggests that the atria are being depolarized by a wavefront moving towards the base of the heart (from inferior to superior; ironically, the "base" of the heart is the superior portion!). This can only happen in a low atrial rhythm or through retrograde conduction from the ventricles through the AV node or an accessory pathway. The interval between the QRS complex and the negative P wave, called the RP interval, is roughly 120 ms.
This rhythm is a short RP tachycardia. The diagnostic differential includes:
- Low atrial tachycardia
- Junctional Tachycardia
- Orthodromic atrioventricular reciprocating tachycardia (AVRT)
- Slow-fast AV nodal reentrant tachycardia (AVNRT)
- During sinus rhythm, the fast pathway excites the ventricles and the slow pathway meets the fast pathway during its refractory period (Figure 1, Panel A).
- If a depolarization wavefront (typically from a premature extrasystole) reaches the AV node at a time where the fast pathway is refractory and the slow pathway is not, it travels down the slow pathway alone (Figure 1, Panel B).
- The depolarization wavefront then meets the fast pathway, which has now recovered from its refractory period, at the distal connection. The arrival of the depolarization wavefront at this junction sends one wavefront to the ventricles through the his-purkinje system and one wavefront towards the atria in a retrograde fashion via the fast pathway (Figure 1, Panel C).
- When this wavefront reaches the slow pathway at the proximal junction, if the slow pathway has recovered from its refractory period, it activates the atria retrogradely and the slow pathway is once again able to propagate the impulse towards the ventricles, creating a cycle of reentry at the AV node (Figure 1, Panel D).
A case series of very slow atrioventricular nodal reentrant tachycardia resembling junctional tachycardia
Clinical and electrophysiologic characterization of automatic junctional tachycardia in adults
- How does the rhythm start? Reentrant rhythms like AVNRT, AVRT, and some atrial tachycardias are usually initiated by a premature extrasystole. Automatic rhythms like some atrial tachycardias and junctional tachycardia usually begin with a "warm-up" period, wherein the automatic focus speeds up to a sustained rate rather than starting suddenly at full speed.
- How does the rhythm behave? Rate variability and slight irregularity is a sign of an automatic rhythm. Reentrant rhythms tend to be regular and do not change much with rate. Episodes of automatic rhythms may terminate quickly, whereas reentrant rhythms are usually more permanent once they're initiated.
- How does the rhythm terminate? In order for a reentrant rhythm to terminate, the circuit through which it propagates needs to be interrupted. Many times, this happens when a premature beat enters the excitable gap (the part of the reentrant circuit with excitable tissue immediately before the head of the depolarization wavefront). This causes two depolarization wavefronts to collide, which terminates the rhythm. Automatic rhythms more often slow down or stop abruptly, allowing the sinus node to regain control of the heart.
- Who is the patient? Junctional tachycardia is more common in young children. Adults very rarely have this arrhythmia. AVRT and AVNRT can happen in both adults and children, so patient history is very important. Does the patient have a known history of WPW syndrome or known dual AV nodal physiology? Atrial tachycardia is more common in "sicker" patients and is usually concomitant with another non-cardiac pathology (sepsis, respiratory distress, etc.).
- Hans favored AVNRT (AtrioVentricular Nodal Reentrant Tachycardia).
- Dr. Smith questioned the diagnosis of AVNRT because of a relatively slower rate than is usually seen with AVNRT (with the usual rate range cited for AVNRT being between 140-280/minute). As a result — Dr. Smith considered JT (Junctional Tachycardia).
- How would you describe the rhythm in Figure-1?
- — HINT: Do you see signs of atrial activity?
.png) |
| Figure-1: I've reproduced the ECG debated on by Hans Helseth and Dr. Smith. |
- Sinus P waves are not present (because there is no upright P wave in lead II ). That said — atrial activity is present, in the form of retrograde P waves (See colored arrows in Figure-2).
- The QRS complex is narrow (because the QRS is not more than half a large box in any of the 12 leads = a QRS ≤0.10 second).
- The rhythm is Regular — at a ventricular Rate of ~115/minute.
- As I note just above — retrograde P waves are present. We know this — because retrograde P waves are negative in the inferior leads (BLUE arrows in Figure-2) — and they are positive in leads aVR, aVL and in lead V1 (PINK arrows in Figure-2).
- And, these retrograde P waves are Related to the QRS complex that precedes them with a constant RP' interval (ie, the distance from the preceding R wave to each retrograde P wave is constant).
- A reentry SVT rhythm (either AVNRT or orthodromic AVRT).
- JT (Junctional Tachycardia).
- Sinus tachycardia is ruled out by lack of an upright, conducting P wave in lead II.
- AFlutter is ruled out because the heart rate of ~115/minute is significantly slower than would be expected for untreated 2:1 AFlutter (that typically manifests a ventricular rate close to ~150/minute [~135-170/minute range] ) — and — there is no sign of 2:1 AV conduction, as would be expected with AFlutter.
- While not impossible — sustained 1:1 ATach is an uncommon rhythm, that would seem less likely to produce negative P waves in the inferior leads with such a long PR interval.
- The usual slow-fast form of AVNRT generally does not manifest the moderately long RP' interval that we see in Figure-2 (in which retrograde P waves are seen to occur past the mid-point of the ST segment). Instead — retrograde P waves with AVNRT are typically either hidden within the QRS complex or occur immediately after the QRS, simulating a pseudo-S wave in the inferior leads.
- Junctional Tachycardia (JT ) — is very uncommon in adults (See below). When JT does occur in adults — in those rare instances in which it manifests retrograde P waves seen after the QRS, the RP' interval will almost always be shorter than that seen in Figure-2 (ie, with an RP' interval seen immediately after the QRS — and not past the middle of the ST segment).
- Bottom Line: The above considerations left me with orthodromic AVRT as the most likely etiology for the rhythm in Figure-2 (ie, with the reason for the longer RP' interval with orthodromic AVRT being the longer distance reentry impulses must travel to complete a reentry circuit that includes the AP [Accessory Pathway], which is located outside of the AV node).
- While true that AVNRT usually manifests a significantly faster rate than 115/minute — there are exceptions in which AVNRT may manifest rates even below the 115/minute of today's case (Higuchi, Scheinman et al — J Cardiovasc Electrophys 33(6): 1177-1182, 2022).
- As in today's case — when the rate of AVNRT is significantly slower than usual for this reentry SVT rhythm — the rhythm may simulate JT.
- The mechanism that may account for AVNRT occasionally occurring at a slower-than-expected rate — is if conduction time over the slower AV nodal pathway is long, and its effective refractory period is short (compared to the ERP of the faster pathway).
-USE.png) |
| Figure-1: I've labeled the "WhoDunnit" ECG debated on by Hans Helseth and Dr. Smith. |
- Sinus rhythm in adults is defined when there are sinus P waves at a heart rate between 60-99/minute in adults.
- The normal AV nodal "escape" rate in adults is between 40-60/minute (and typically between ~50-80/minute in children).
- An accelerated Junctional Rhythm in adults is defined as a junctional rhythm that is faster than the normal "escape" rate (ie, over 60/minute) — but less than 100/minute.
- JT (Junctional Tachycardia) — is defined as a junctional rhythm that is ≥100/minute.
- Junctional Ectopic Tachycardia (JET ) — is almost exclusively seen in infants and children. There is both a congenital form (CJET) — and a post-operative form (POJET), with this latter form usually occurring within 72 hours after operation for correction of congenital heart defects — and usually being self-limited within several days of its onset.
- CJET is much less common than POJECT — with early recognition of this congenital form essential because of its high morbidity and mortality, as well as the difficulty with effective treatment.
- NOTE: Beyond the pediatric age — true JT is not common in adults (Ashraf & Goyal — StatPearls, 2023).
- True automatic Junctional Tachycardia (ie, JET, as above) — is primarily a pediatric arrhythmia.
- Most of what has previously been classified as JT in adults — probably was either slower-than-expected AVNRT or on rare occasions, infra-atrial reentrant tachycardias (ie, in which the His or hemibranches serve as part of the reentrant circuit).
- Rather than an automatic, paroxysmal rhythm — most faster junctional rhythms in adults as best thought of as accelerated junctional rhythms, in that they are non-paroxysmal, and typically the result of "something else" (ie, sepsis, electrolyte disturbance, acid-base disorder, or otherwise "sick patient" — Digoxin toxicity — post-operative state). These rhythms typically resolve if the "something else" can be identified and treated.
- While not strictly limited to heart rates of ≤100/minute — these faster junctional rhythms are generally not nearly as fast as true paroxysmal, automatic JT (ie, I still look for "something else" if I encounter a junctional rhythm up to ~110-120/minute — with best treatment often being treatment of the underlying disorder rather than rate-slowing medication).
- Although rare in adults — true paroxysmal JT is important to rule out in problematic regular SVT cases that are referred to EP Cardiology, because longterm treatment is different than treatment of AVNRT and AVRT (ie, paroxysmal JT is much less likely than reentry SVTs to respond to ablation — and it carries a much higher risk of AV block if ablation is attempted).
- The mechanism of JT is increased automaticity arising from the AV Node. This differs from the reentry mechanism associated with AVNRT and AVRT. This difference in mechanism influences therapeutic decision-making.
- True paroxysmal ectopic junctional tachycardia (ie, JET) — is essentially a pediatric rhythm. In infants and young children — JET may be congenital, but it most commonly occurs as a self-limited arrhythmia in the post-operative state following surgery for congenital heart disease.
- Accelerated junctional rhythms may occur in adults — but they are not common. Think of some underlying cause if seen — with the "good news" that much of the time accelerated junctional rhythms will resolve if their cause is identified and treated.
- Rather than artificial distinction by a rate over or under 100/minute between "accelerated" junctional rhythms vs junctional "tachycardia" — I favor the following concept: i) True paroxysmal JT in adults is rare (and capable EP cardiologists will identify those rare cases among the regular SVTs referred to them); and, ii) Almost all of the faster junctional rhythm cases I have seen up to rates of ~120/minute — will be the result of "something else" — with BEST initial management typically consisting of trying to find and "fix" that something else causing this rhythm.
- Although the usual rate of reentry SVT rhythms is ≥140/minute — on occasional, AVNRT or AVRT may be seen with heart rates of 110/minute or less.










-USE.png)


-USE.png)
-USE.png)